What Is Apgar Score and What Is Its History
The Apgar scale is an assessment method that unites newborns from all over the world.
Briefly About the Baby’s Apgar Score
You might not need to delve into all the historical details of the Apgar score right now. Here's a brief overview:
The Apgar score is a scoring system used to assess the condition of a newborn. The assessment is based on five criteria:
- Skin color,
- Pulse rate,
- Reflex irritability grimace,
- Muscle Tone,
- Respiratory effort.
Each parameter receives a score from 0 to 2.
The total score is calculated at 1 minute and 5 minutes after birth. 7–10 points indicate that the baby does not need special observation. 4–6 points mean the doctors should provide a more intensive medical attention. 0–3 points is considered a low Apgar score. It indicates that the emergency care is required.
The Apgar score is a method of assessment endorsed by the American College of Obstetricians and Gynecologist and the American Academy of Pediatrics [5].
If you're interested in the history of the Apgar score or more detailed information, read on.
Introduction
Would it have been great to be born in the 19th century? Scientific progress, steam engines, the rise of new social theories. It seems like a romantic and beautiful era of great people and achievements.
However, this romantic view hides one very unpleasant detail. Had we been born in the 1860s in the British Empire, only three quarters of us would have made it to the 1870s [1]. The level of medical care at that time made childbirth a very risky procedure.
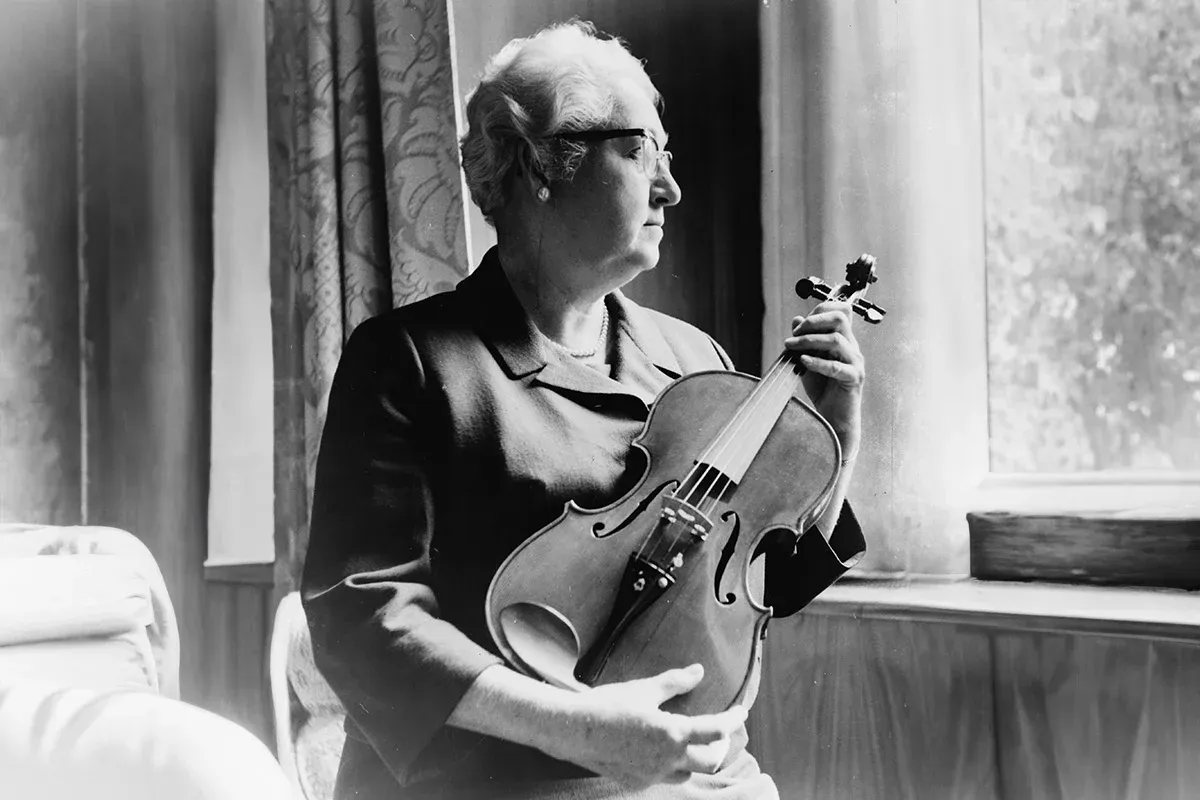
History and Motivation Behind the Virginia Apgar Scores
One article about the life of American anesthesiologist Virginia Apgar suggests that her primary motivation for creating the famous scoring system was the high infant mortality in the United States in the 1930s [2].
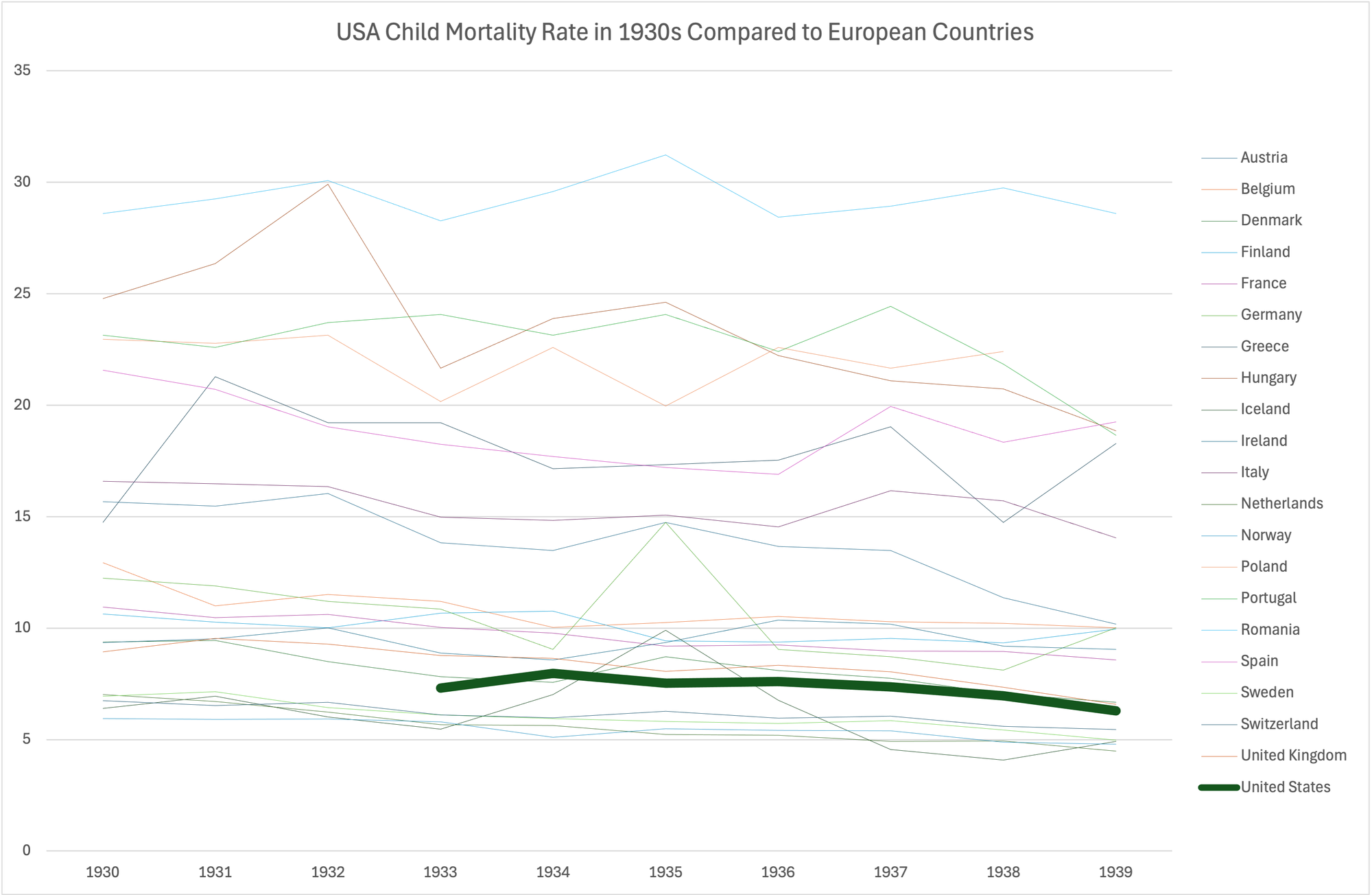
I was unable to verify this claim. Comparative data on infants in the 1930s is scarce, but information from the late 1940s and early 1950s shows that the situation wasn’t all that terrible. In 1950, the U.S. lagged just 1% behind the leader, Sweden, while conditions in Poland were four times worse [3].
In the 1930s, the data for children under five in the U.S. did not reveal any serious anomalies compared to European countries. The results were closer to the leading ones.
Instead of speculating, we can listen to the creator of the APGAR test herself. Here’s what Virginia wrote in her article “The Newborn (Apgar) Scoring System. Reflections and Advice” [4]:
The original intention of establishing a scoring system was to predict survival, to compare several methods of resuscitation which were in use at the time, and through the infant's responsiveness after delivery, to compare perinatal experience in different hospitals. The influence of various obstetrical practices such as induction of labor, elective ce- sarean section and maternal anesthesia and analgesia might well be reflected in the score. It was furthermore hoped that the scoring system would ensure closer observation of the infant during the first minute of life. The value of the system for neonatal research and for predicting neuromuscular deficit in early childhood was demonstrated later.
Today, the Apgar score is a method for assessing the newborn's condition and deciding whether neonatal resuscitation is needed.
Virginia Apgar presented her standardized assessment at a joint meeting between the International Anesthesia Research Society and the International College of Anesthetists [5]. A year later, the article “A Proposal for a New Method of Evaluation of the Newborn Infant” was published, introducing the Apgar score to the public.
The article not only described the signs and included brief commentary but also featured a comprehensive study listing Apgar tests for babies born in different circumstances: head presentation, breech, cesarean section, and others. It was the population-based cohort study that assisted Apgar score.
Baby’s Apgar Score Indicators
Here’s a list of the indicators from Wikipedia:
- Skin color,
- Pulse rate,
- Reflex irritability grimace,
- Muscle Tone,
- Respiratory effort.
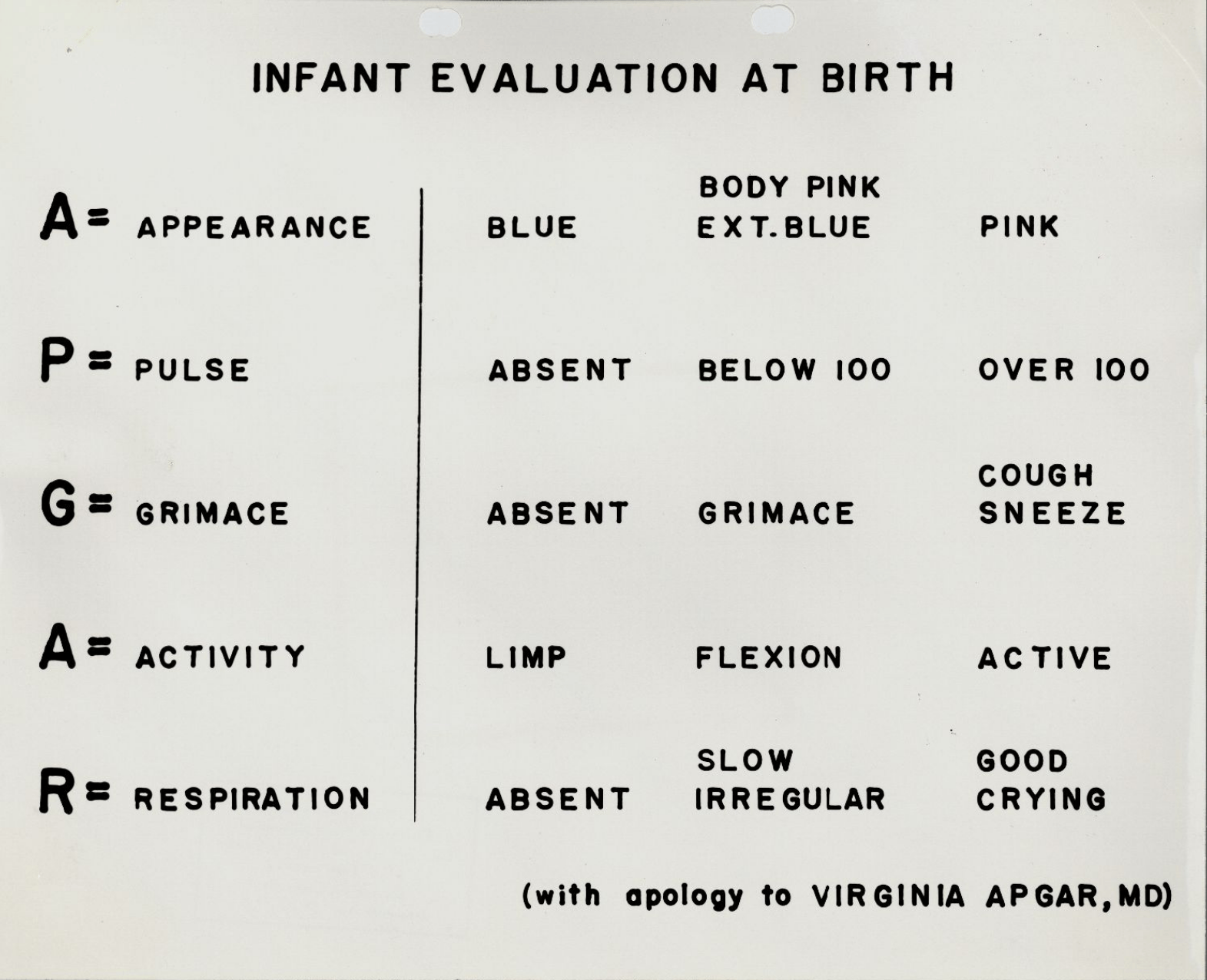
For better remembering, a mnemonic was introduced in 1961 by Joseph Butterfield. The backronym is APGAR, standing for:
- A — Appearance, indicating skin color.
- P — Pulse, or baby's heart rate.
- G — Grimace, or the response to stimulation.
- A — Activity, meaning muscle tone and movement.
- R — Respiration, or breathing.
In Virginia Apgar’s original article, the indicators were ordered by importance as follows:
- Pulse,
- Respiration,
- Grimace,
- Activity,
- Appearance.
I didn't discover any evidence that Virginia agreed with Joseph Butterfield’s mnemonic. However, it seems to be in a wide use. Interestingly, birth weight and height, parents’ favorite measurements, are not part of the Apgar score, although this trio of numbers is typically what excites new parents.
Potential Scores for Apgar Indicators
Each indicator can be scored from 0 to 2. The higher the score, the better. Low Apgar scores might be a reason for medical intervention. Below are the indicators and their corresponding scores:
Indicator | 0 points | 1 point | 2 points |
|---|---|---|---|
Skin color | Blue or pale | Pink body, blue limbs | Completely pink |
Breathing | Absent | Irregular breathing, weak cry | Normal, loud cry |
Heart rate | <60 | <100 | >100 |
Response to stimulation | No response | Grimace or weak response | Movement, cough, sneeze in response to stimuli |
Muscle tone | Limp, no movement | Weak flexion of limbs | Active movement |
As you might have observed from the table, the more Apgar scores a newborn gets, the better is the condition.
Evaluation Procedure in the Delivery Room
In the article “The Newborn (Apgar) Scoring System. Reflections and Advice” the following tips for using the Apgar scoring are provided:
It is strongly advised that an observer, other than the person who delivers the infant, be the one to assign the score.
An automatic method of announcing the passing of 60 seconds is recommended.
Although mortality and the presence of significant neurologic damage correlate better with the five-minute than the one-minute score, the one-minute score should nevertheless be retained. It is essential to observe the infant from the moment of birth in order that prompt treatment can be given if necessary. Nine months' observation of the mother surely warrants one-minute observation of the baby.
Thus, the result of the assessment is two numbers. For example, 7-9 means that at 1 minute after birth, the baby scored 7 points, and at 5 minutes, they scored 9 points. Most babies have lower Apgar scores at one-minute measurement and higher five-minute Apgar scores.
Actions Based on Baby’s Apgar Scores
Based on the five-minute Apgar score measures, newborns fall into one of three groups:
- 7–10 points — a baby who doesn’t require special observation.
- 4–6 points — a baby who needs observation. Moderately abnormal baby's Apgar score.
- 0–3 points — a baby who requires immediate medical care or maybe even resuscitation efforts.
Virginia Apgar noted [4] that if initial resuscitation is visibly needed immediately after birth, doctors should not wait for a minute to conduct the first assessment, but should act without delay.
Impact of High, Moderate or Low Apgar Score on the Baby's Development
I'll just quote a 2001 article that summarizes 50 years of using this evaluation method [8]:
The value of the Apgar score has become controversial because of attempts to use it as a predictor of the neurologic development of the infant, a use for which it was never intended. For example, the use of the Apgar score to identify birth asphyxia is a misapplication, since conditions such as congenital anomalies, preterm birth, and administration of drugs to the mother can result in low scores that are not reflective of asphyxia.
The purpose of this excellent list is not to predict a baby’s life-long development or future health, but to help health professionals quickly orient themselves and improve the chances of survival for the baby. This is why the Apgar score is applied to every baby born in a hospital.
Conclusion
The Apgar score is a proven tool for saving newborns’ lives. It didn’t play a role in reducing worldwide infant mortality from 50% to 5%, but it does play a first violin in the next step — reducing mortality from 5% to 0.5%.
Was it interesting to know how a doctor evaluates the health status of a newborn on the Apgar scale? Subscribe to the “So List” blog — there are many more amazing lists and checklists in the world. You’ll also learn how to solve many issues with these simple yet powerful tools.
List of Links
[1] “Child mortality rate, 1841 to 2022” from “Our World in Data” website
[2] “Virginia Apgar (1909-1974): The Mother of Neonatal Resuscitation” from “PubMed Central” website
[3] “Infant mortality rate” from “Our World in Data”
[4] Virginia Apgar, “The Newborn (Apgar) Scoring System. Reflections and Advice”
[5] “Apgar score” from Wikipedia
[6] Virginia Apgar, “A Proposal for a New Method of Evaluation of the Newborn Infant”
[7] “Letter from L. Joseph Butterfield to Virginia Apgar” from “Five College Compass” website
[8] Brian M. Casey, M.D., Donald D. McIntire, Ph.D., and Kenneth J. Leveno, M.D., “The Continuing Value of the Apgar Score for the Assessment of Newborn Infants”